With Dr. Doodes
 Can I get a filling done while pregnant / lactating? When you’re pregnant you can look forward to being showered with lots of advice. However, you’re unlikely to hear someone suggest completing dental work. For a long time the thought was; postpone dental work or you’ll harm the baby. This opinion is not supported by data. In fact, physicians fully recognize the importance of oral health. The American College of Obstetricians and Gynecologists (ACOG) recommends patients to complete all necessary dental work, even while pregnant, including any necessary x-rays, fillings, root canal treatments, extractions and crowns. ACOG and the American Dental Association (ADA) agree that untreated oral infections pose a risk to the mother and fetus [1].
Can I get a filling done while pregnant / lactating? When you’re pregnant you can look forward to being showered with lots of advice. However, you’re unlikely to hear someone suggest completing dental work. For a long time the thought was; postpone dental work or you’ll harm the baby. This opinion is not supported by data. In fact, physicians fully recognize the importance of oral health. The American College of Obstetricians and Gynecologists (ACOG) recommends patients to complete all necessary dental work, even while pregnant, including any necessary x-rays, fillings, root canal treatments, extractions and crowns. ACOG and the American Dental Association (ADA) agree that untreated oral infections pose a risk to the mother and fetus [1].
Is fluoride ok while pregnant? Yes. The American Dental Association recommends all humans with teeth use a small amount of fluoride containing toothpaste twice daily for 2-3 minutes to promote strengthening of the tooth surface. Toothpaste is not absorbed by the body in any significant way other than on the tooth surface.
Left: My wife and OB-GYN physician carrying our 1st child.
What about local anesthesia? We are interested in reducing your stress; so we use local anesthetic to eliminate pain. We use the minimum amount necessary as is endorsed by the ACOG even while pregnant or lactating[1].
What dental problems can I expect while pregnant?
Usually none, but the most common dental problems associated with pregnancy are [2]:
- Enamel erosion due to morning sickness. Frequent exposure to stomach acid can erode enamel. Rinsing your mouth and using fluoride mouthwash will help strengthen the tooth surface.
- Gum inflammation. Hormonal changes can promote red, sore gums. Brush twice daily and floss to reduce swelling.
- Dry mouth. Rare, but increases risk of tooth decay (caries). See my DHM article on dry mouth on our website.
- Tooth mobility. Seldom seen, but increased inflammation can lead to softer bone around the teeth and limited mobility. Resolves after pregnancy
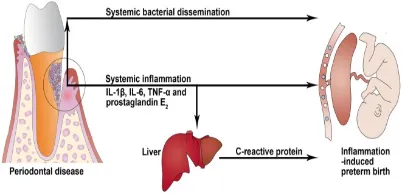
- Periodontitis: Untreated gingivitis (inflammation of the gums) can progress into periodontitis, which is irreversible bone loss around teeth and remains the #1 cause of tooth loss in adults in the USA.
- Benign oral lesions (Pyogenic granuloma). Small vascular mass typically appearing on the anterior
Can I get my teeth whitened during pregnancy? While there is no data to suggest that tooth whitening is detrimental for the developing fetus, we still advise to pass on whitening until after the birth.
Should I get my deep cleanings before I give birth? ‘Last-minute’ treatment for a chronic problem such as gum disease may not be effective at preventing low birth weight (LBW) [3,4] but may be helpful prior to pregnancy.
Right: How periodontal disease is thought to affect the fetus.
How does dental care affect pregnancy outcomes?: While prenatal dental care has not been shown to improve birth outcomes [3,4], there is ample evidence that improved oral health may reduce transmission of decay causing bacteria to the infant and promote a sustained reduction in tooth decay risk [5,6,7].
Conclusion: Dental care is important throughout life; that doesn’t stop during pregnancy. Follow the recommendations of the experts at the ACOG and follow-through with all non-elective dental work for optimal maternal and fetal health.
References:
- https://www.acog.org/-/media/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/co569.pdf
- Systemic alterations and their oral manifestations in pregnant women. J Obstet Gynaecol Res. 2017 Jan;43(1):16-22. Silva de Araujo Figueiredo C, Gonçalves Carvalho Rosalem C, Costa Cantanhede AL, Abreu Fonseca Thomaz ÉB, Fontoura Nogueira da Cruz MC.
- Scaling and root planing performed on pregnant women with mild to moderate periodontal disease is not efficacious in reducing preterm birth, low birth weight, or other poor pregnancy outcomes. J Evid Based Dent Pract. 2012 Sep;12(3):135-7. Dasanayake AP
- The effectiveness of periodontal disease treatment during pregnancy in reducing the risk of experiencing preterm birth and low birth weight: a meta-analysis. J Am Dent Assoc. 2010 Dec;141(12):1423-34. Uppal A et al.
- The effect of caries-preventive measures in mothers on dental caries and the oral presence of the bacteria Strep. Mutans and Lactobacilli in their children. Arch Oral Bioll 1984;29:879-83
- Effectiveness of a caries preventive program in pregnant women and new mothers on their offspring.Int J Paediatr Dent. 2001 Mar;11(2):117-22. Gomez SS1, Weber AA.
- An early oral health care program starting during pregnancy: results of a prospective clinical long-term study.Clin Oral Investig. 2010 Jun;14(3):257-64. Meyer K et al.,
Regardless, bottled water has become a lifestyle choice for many people and it’s here to stay. According to the International Bottled Water Association, sales in the US reached a $14.2 billion in 2015 continuing the steady rise seen for decades [1].
Where is bottled water from? Sources are typically natural springs, but some of the biggest names supply filtered public water. Each of the products has small variations in mineral content, and pH [2].
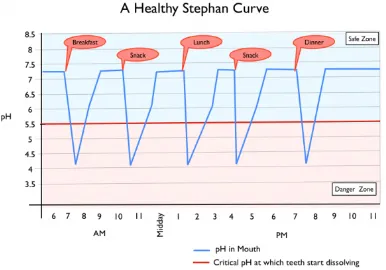
What is pH? pH is a measure of acidity. A lower pH means the substance is more acidic, and a higher pH means it is more alkaline (see image on right). Importantly, the pH scale is logarithmic, meaning that a liquid with a pH of 5 is ten times more acidic than a liquid with a pH of 6.

Left: Note how mealtimes initiate a drop in pH. Now consider how snacking will keep the pH low – potentially all day [3]. To help neutralize the acidity of meals, choose beverages that are at a pH of 5.5 of higher.
Is an alkaline water (or diet) healthier? The pH of the blood is tightly regulated by your lungs, kidneys and blood buffers to keep your pH within a healthy range of pH 7.35-7.45. Deviating above that range may cause symptoms of alkalosis including irritability, muscle twitching, muscle cramps; this condition requires a physician to diagnose and treat.
No reputable published data supports ‘alkaline diets’ [4]. Don’t try to fight your body’s pH – it is a highly regulated system and doesn’t require or benefit from attempts to alter it. As for your mouth, a water that is neutral or slightly alkaline would help neutralize the acids produced by bacteria on the teeth and would therefore help to reduce the time your oral pH is below the critical pH 5.5.
How acidic is my bottled water? To test the pH of common bottled waters we used a calibrated glass electrode pH meter to test 8 different brands of still bottled water. We also tested tap water and filtered tap water. Each sample was tested at room temperature and the test was repeated three times in series. The pH meter was rinsed between samples and recalibrated after each series. Mean averages of data shown. No statistical analysis were performed. Here are our results:
If you’re worried about the acidity of bottled water just stick with tap water. Well water – or from your city – is often closer to neutral than bottled water. The standards for purifying tap water are stringent and well regulated compared to those that govern bottled water [5]. So, your bottled water may or may not be as pure as your own tap water.
What about fluoride? Fluoride works by increasing the acid resistance of your teeth. It works by being substituted with the less acid-resistant calcium ion in the major component of tooth enamel, hydroxyapatite. This simple substitution reduces decay rates and is the reason why fluoride concentrations in most municipal supplies have fluoride concentrations adjusted for optimal benefit. Many bottled waters have minimal fluoride content. Water that is low in fluoride and mildly acidic will push your enamel to become weaker.
If bottled water is your choice, choose brands that are best for your teeth: If we don’t have the results you need, type “brand X pH” and Google will give you the pH. Our results correlated well with online data. Find a bottled water that is pleasing to your taste and has a near neutral pH. And remember, that the small amount of fluoride in tap water – and especially toothpaste – is beneficial to teeth of all ages [6,7].
Sincerely,
Dr. Doodes
References:
- //www.bottledwater.org/public/BWR_Jul-Aug_2016_BMC%202015%20bottled%20water%20stat%20article.pdf#overlay-context=economics/industry-statisticsnjnjughruruiwid9edib9gi90586989tj
- //www.ada.org/en/member-center/oral-health-topics/bottled-water
- Advances in Remineralization for Early Carious Lesions: A Comprehensive Review. S Jefferies et al., April 2014, Compendium of Continuing Education in Dentistry
- Systematic review of the association between dietary acid load, alkaline water and cancer. Fenton TR, et al., BMJ Open. 2016 Jun 13;6(6
- Critique of the review of ‘Water fluoridation for the prevention of dental caries’ published by the Cochrane Collaboration in 2015. Rugg-Gunn AJ et al., Br Dent J. 2016 Apr;220(7):335-40.
- Water fluoridation for the prevention of dental caries. Iheozor-Ejiofor Z et al., Cochrane Database Syst Rev. 2015 Jun 18;(6)
© Paul Doodes DDS PhD. All rights reserved.
Why do we need to brush our teeth? Most of your body’s surfaces shed, including your hair, skin, intestinal lining and nails; but teeth are different… their surface doesn’t shed. Teeth’s non-living surface is hard and has little capacity for repair. Because of this, teeth need mechanical cleansing. Without brushing and flossing, bacteria on the teeth produce acid every time you eat sugar or simple carbohydrates eventually causing cavities.
What is available? The choice of toothbrushes at a regular supermarket is bewildering. The market can be broken up into three general categories:
(1) Manual brushes
(2) Electric brushes (disposable battery)
(3) Electric brushes (rechargeable battery built in)
Manual toothbrushes are, despite their humble prices and modest technology, quite effective when used with good technique, gently for 2-3 minutes for 2-3 times a day.
The low power, battery operated electric toothbrushes are popular due to their apparently modern design and low price. However, they are offer no improvement in plaque and tartar/calculus reduction vs. manual toothbrushes. Their efficacy is limited by their low power and therefore limited rotational speed of the brush head.
The electric toothbrushes that offer a benefit to consumers in terms of plaque and calculus reduction are divided into the ultrasonic (e.g. Sonicare™) type brushes and the high-powered rotational head type brushes (e.g. Oral-B). The ultrasonic type brushes vibrate the head up to 31,000 times a minute, literally breaking apart bacterial colonies. The powerful rotations of an Oral-B physically break off plaque from the tooth, similar to a manual toothbrush, but with greater effectiveness. This data is supported by a dentist-blinded clinical trial that showed “Oral-B Triumph with its rotation-oscillation action was significantly more effective in single-use plaque removal than Sonicare Elite 7300” [Biesbrock, AR et al.].
In 2003, the prestigious Cochrane reviews critically examined data from 29 well-designed studies looking at toothbrush efficacy. They concluded that the electric toothbrushes “Consistently provided a statistically significant, although modest, clinical benefit over manual toothbrushes in reducing plaque and gingivitis” [Neiderman et al].
A recent, comprehensive study by Klukowska et al. conclude that after a dentist-blinded study of Sonicare and Oral-B’s latest brushes that the Oral-B “Demonstrated statistically significantly greater reductions in whole mouth plaque at Weeks 6 and 12, as well as significantly greater gingivitis reductions over the long-term (12 weeks), compared to the new sonic toothbrush”.
What are my recommendations? With good technique, soft bristled manual brushes work well. However, most people don’t brush for 2-3 times a day for 2-3 minutes with ideal technique. This is why most people would benefit from a more effective brush that helps you to time your brushing too!
Perhaps unsurprisingly, I have a manual brush, a Soniare and an Oral B. Any of which will work well. However, after reading enough large, well designed, financial-conflict free studies with similar results, I am confident the Oral-B will provide the best plaque and calculus removal (this is why we have them available in the office).
Remember, all toothbrushes lose their plaque fighting ability as they age, so be sure to keep a stock of fresh brush heads / brushes at home and replace them every 3-4months or when they frey [ADA]
If you have any questions, please feel free to email me at doodesdds@gmail.com Who knows, maybe your question will be the subject of another edition!
References
Biesbrock, AR; Bartizek, RD; Walters, PA; Warren, PR; Cugini, M; Goyal, CR; Qaqish, J (2007). “Clinical evaluations of plaque removal efficacy: an advanced rotating-oscillating power toothbrush versus a sonic toothbrush”. J Clin Dent. 18 (4): 106–11.
Niederman R, et al. J Am Dent Assoc. 2003 Sep;134(9):1240-4. Manual vs powered toothbrushes: the Cochrane review.
Klukowska M, et al., A randomized 12-week clinical comparison of an oscillating-rotating toothbrush to a new sonic brush in the reduction of gingivitis and plaque. J Clin Dent. 2014;25(2):26-31.
ADA://www.ada.org/en/about-the-ada/ada-positions-policies-and-statements/statement-on-toothbrush-care-cleaning-storage-and-
© Paul Doodes DDS PhD. All rights reserved.
What causes bad breath?
Many things contribute to foul breath including (1):
Bacteria:
The mouth is a perfect breeding ground for many bacteria, some of which produce the volatile sulphur compounds (VSC’s) that are responsible for the most offensive odors. The bacteria often inhabit the back of the tongue and throat, areas that are seldom cleaned effectively.
Dry mouth / Dehydration:
As discussed in a previous DHM, a slightly dry mouth allows some particularly offensive bacteria to flourish – and also decay rates to soar.
Gum Disease:
The sticky plaque that is responsible for gum disease (periodontal disease) is also responsible for an increase in foul odor.
Food:
Sadly, those salad onions at lunch will follow your breath for many hours. And your coffee, garlic… the list goes on.
Smoking:
Obvious to anyone within 6 feet of you for hours and hours after you light up.
Medical Conditions:
After we have eliminated other sources of malodor, we begin to consider medical conditions such as gastric reflux, sinus infections, diabetes or even liver or kidney disease.
Dirty removable appliances:
Your occlusal guard (see previous DHM article), dentures, partial dentures, snore-guard, Invisalign trays or retainers all can harbor bacteria. Gentle daily brushing with water and weekly cleaning with a cleansing tablet help keep things fresh.
What to do?
Good oral hygiene is an essential first step: Brushing thoroughly, gently, and consistently will clean most of your teeth, but only flossing will clean in between your teeth. Together, this will loosen bacteria off the teeth; tongue scraping and mouthwash will help to clean the back of the throat and remove many of the worst bacteria. Less odorous food choices, good hydration, stopping smoking addressing dental decay and gum disease will reduce odors too.
What mouthwash will help?
Some mouthwashes will mask smells briefly, but as many contain alcohol, Many products are effective at reducing bad breath (2). The most effective ones will not simply mask an odor, but kill the most offensive odor molecules and bacteria where they live – at the back of the tongue and throat (3,4,5).
So what works?
Funny you should ask. After years of looking into this common problem, using many formulations, reading articles in the dental press and hearing from patients, I’ve come to recognize a class of mouthwash containing chlorine dioxide (ClO2) as the most effective (3,4,6). Chlorine dioxide mouthwashes readily oxidize (i.e. destroy) the common odors and bacteria in the mouth. Chlorine dioxide has been used for decades to disinfect and deodorize municipal water supplies worldwide.
The first chlorine dioxide mouthwash was developed in 1992 by a periodontist called Dr. Richter (6). He developed a regimen of twice daily tongue scraping and gargling to almost eliminate halitosis. His patent is unique as it uses an activated chlorine dioxide compared to other more stable (read: less active) formulations. His ‘ProFresh’ formula was also shown to help remove the bacteria on teeth that cause gum disease. It works almost instantly. It’s gentle on the mouth and helps breath and reduces plaque!
Yes, I’m a fan. The downside? It does not taste delightful like other mouthwashes; it tastes like tap water. But don’t be fooled, you’ll notice how effective it is instantly. I’ve been using it daily for over a year and after suggesting it to many patients we are now stocking it in the office.
Ask me if you have any bad breath questions, and feel free to share this article!
References:
- Braz Oral Res. 2011 Sep-Oct;25(5):466-71.Halitosis: an overview of epidemiology, etiology and clinical management. Rösing CK, Loesche W.
- Int J Dent Hyg. 2016 May;14(2):117-23. The effect of different mouth rinse products on intra-oral halitosis. Erovic Ademovski S1, Lingström P2, Renvert S1,3,4.
- Isr J Dent Sci. 1989 Oct;2(3):142-7. Use of a metastabilized chlorous acid/chlorine dioxide formulation as a mouthrinse for plaque reduction. Goultschin J1, Green J, Machtei E, Stabholz A, Brayer L, Schwartz Z, Sela MN, Soskolne A.
- J Oral Biol Craniofac Res. 2016 Jan-Apr;6(1):54-8. Effect of Aloe vera, chlorine dioxide, and chlorhexidine mouth rinses on plaque and gingivitis: A randomized controlled trial. Yeturu SK1, Acharya S2, Urala AS3, Pentapati KC4.
- Braz Oral Res. 2016 Aug 22;30(1):e71. Self-reported halitosis and associated demographic and behavioral factors. Milanesi FC1, Kauer B1, Wagner TP1, Daudt LD1, Haas AN1
- Diagnosis and Treatment of Halitosis Jon L. Richter, DMD, PhD Compendium of Continuing Education in Dentistry, April 1996.
© Paul Doodes DDS PhD. All rights reserved.
Taking a look along the aisles at the supermarket and you’d be forgiven for thinking that there’s a special toothpaste for just about everybody. This is all a little odd considering that toothpaste really isn’t much more effective than simply using a toothbrush alone – the mechanical brushing is what’s most important (1). However, toothpaste provides a great degree of comfort, a minty fresh feeling, and a small amount of fluoride that will help strengthen slightly weaker areas of the teeth (2).
The wealth of toothpastes can be divided into several categories of toothpaste including ‘natural’, whitening, sensitive, high fluoride, tartar control and children’s toothpaste. Let’s take a quick look at each:
Natural Toothpaste
The term ‘natural’ is not legally defined, and usually doesn’t mean organic. Generally, natural toothpastes do not contain artificial sweeteners, dyes or flavors, but some products do contain sodium lauryl sulfate, a foaming agent that can – in some people – cause mouth sores. Some natural products contain added fluoride. Some natural toothpastes contain glycerin, which can coat your teeth and prevent them from absorbing minerals.
Whitening Toothpastes
Whitening toothpastes typically contain either a bleaching agent or an abrasive, such as silica or both. The bleaching agents commonly used are peroxide or sodium tripolyphosphate, the same reagents used to whiten teeth however, with only a few minutes exposure, there is insufficient time – and concentration – to whiten teeth. These toothpastes have widespread appeal, but are for most people unnecessarily abrasive. Whitening treatments whiten teeth from the outside in, whitening toothpastes simply aggressively scrub the outer surface of teeth.
Sensitivity Control Toothpastes
Many patients complain of mild, brief sensitivity to hot or cold foods and liquids. This common problem has been helped considerably by the creation of toothpastes that contain either potassium nitrate or strontium acetate/chloride to mitigate that sharp pain. They take about 2 weeks to work, but are a first line of defense against sensitivity. In-office desensitizers work by the same mechanism, but have greater efficacy vs. over the counter sensitivity toothpastes (3).
High Fluoride Toothpastes
Almost all toothpastes in the US contain fluoride. Fluoride has been shown conclusively to reduce decay rates when used in concentrations found in modern toothpastes (2). Many adults benefit from high-fluoride toothpaste, especially if they are taking medications that cause their mouth to be dry, or when they have health conditions that make them more vulnerable to tooth decay. These products are prescription only and can give a boost of fluoride to help strengthen weaker areas before they cavitate (i.e. form a cavity). If you suffer from dry mouth, or have a high-decay rate, we’ll be happy to discuss high-fluoride options.
Tartar Control Toothpastes
Some products claim to help prevent tartar (also known as calculus, or hard build-up)(4). These products are sometimes simply more abrasive, but one product – Colgate Total – contains Triclosan, an effective antimicrobial, that effectively reduces plaque and tartar. It has been banned from use in soaps (5), but due to it’s efficacy in plaque removal (6) it’s been allowed by the FDA to remain in toothpastes.
Childrens Toothpastes
The American Academy of Pediatric Dentists now recommends everyone of every age to use a fluoride toothpaste (7)(recall a grain of rice sized portion for youngsters), these products are simply for personal preference. A wide variety of colors, tastes and packages emblazoned with their favorite characters helps encourage regular brushing.
In conclusion, the frequency and technique of brushing is what matters most. Use an ADA Approved product (8), a soft toothbrush for 2-3 minutes, 2-3 times a day for the best results. Be gentle. Be thorough. Be consistent.
Share if you care! Please feel free to share this or any Dental Health Matters article and if you have any questions, please feel free to email me at doodesdds@gmail.com Who knows, maybe your question will be the subject of another edition!
References:
- Valkenburg C. et al., J Clin Periodontol. 2016.Does dentifrice use help to remove plaque? A systematic review.
- Walsh T. et al., Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents.Cochrane Database Syst Rev. 2010 Jan 20;(1)Cochrane Database Syst Rev. 2010 Jan 20;(1):CD007868
- Charig et al., Mechanism of action of a desensitizing fluoride toothpaste delivering calcium and phosphate ingredients in the treatment of dental hypersensitivity. Part II: comparison with a professional treatment for tooth hypersensitivity. Compend Contin Educ Dent. 2009 Nov-Dec;30(9):622-4, 626,
- Spivakovsky S. et al., The effect of anti-plaque agents on gingivitis. Evid Based Dent. 2016 Jun;17(2):48-9.
- //www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm517478.htm 2016
- Trombelli L et al., Efficacy of triclosan-based toothpastes in the prevention and treatment of plaque-induced periodontal and peri-implant diseases. Minerva Stomatol. 2013 Mar;62(3):71-88.
- //www.aapd.org/resources/frequently_asked_questions/#320
© Paul Doodes DDS PhD. All rights reserved.
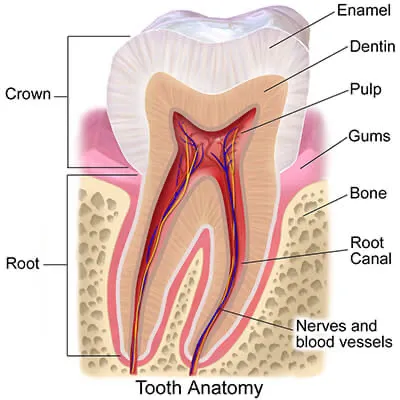
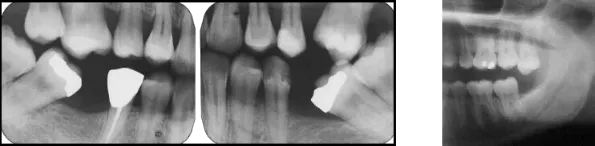
The crown is the white part of the tooth that is visible in your mouth. More accurately, it is the outer coating of hard enamel over the slightly softer inner dentin that makes up the root and middle layer of the tooth (below left).
Do I need a new crown?
Teeth endure significant wear and tear from eating, grinding and from bacteria that reside on and in between teeth – an area the toothbrush bristles simply don’t reach. When tooth is missing structure or exhibits damage from either decay or a large – especially an old metal – filling a crown is needed. Metal fillings are always wider at their depth than the surface, which when large enough, undermines the strength of the cusps. It is common for us to see large metal fillings with hairline fractures at the edges or with entire sections of tooth missing around the filling (Above, middle: note missing cusp and fracture line on right side of tooth). It is even the case that an unrestored tooth may exhibit signs or symptoms of cracking as the crack enters the highly sensitive pulp of the tooth. The tooth in the above right image has a large metal filling and the arrows indicate areas of visible cracking. Without the protection of a crown or an onlay to encapsulate the tooth, these cracks will propagate deeper into the tooth. If you are lucky you’ll just lose a cusp (middle image) if you’re unlucky you’ll crack the tooth severely and you’ll need an extraction and implant as well as the crown that was originally indicated. Early intervention is key.
What is a crown made of these days?
Dental materials have improved dramatically. The traditional gold crown is still an excellent choice, especially for molars, but with the cost of gold both high and unpredictable it’s seldom the 1st choice. Similarly, the traditional porcelain fused to metal (PFM) has declined in popularity as stronger, more life-like options such as Emax (Lithium disilicate) and Zirconia crowns have become available (See below. Image from Ref 1).
The esthetics of Emax and Empress materials is simply excellent. Zirconia crowns with their natural look and high-strength, finally offer an attractive material choice for those who grind their teeth. However, no material is perfect; each material has its strengths and limitations and material choice will depend on the location of the tooth, the neighboring and opposing teeth materials and the wear of other teeth (i.e. if the patient grinds their teeth at night)(Ref. 2,3,4). Staying current with the latest peer-reviewed articles and years of experience will allow us to evaluate if you need a crown, and what material is likely to give you the best long-term result. Whichever material is best for you, you can be sure that with routine care, these materials will give you years of comfortable, functional, beautiful service.
If you have any questions, please don’t hesitate to contact our office.
References:
- Dental Economics: Which indirect restorations do dentists want in their own mouths? GJ. Christensen, DDS, MSD, PhD.
- Dent Mater. 2013 Dec;29(12):1201-8. Edge chipping and flexural resistance of monolithic ceramics.
- J Prosthodont Res. 2013 Oct;57(4):236-61.Current status of zirconia restoration
- J Prosthet Dent. 2014 Jul;112(1):22-30. doi: 10.1016/j.prosdent.2014.01.005. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: a systematic review.
Do I need it? Some signs that teeth may not be properly aligned can include jaw pain, over or underbite, protrusion or crowding (overlapping) of teeth, extra or uneven spaces between teeth, and difficulty with brushing or flossing which can lead to cavities and even gum disease. Orthodontic treatment is often recommended to correct these issues to help achieve optimal oral health. Invisalign also works well to correct problems on patients who previously had braces [1].
How is it done? During an initial Invisalign visit we first examine your mouth completely starting with an examination of your lips, cheeks, tongue, and gums for signs of irregularities, infection… or worse. We then ensure your teeth are healthy – visually and with radiographs – to check completely for cavities or failing restorations. We then take a series of photos and impressions to comprehensively record your case We then write a prescription and once a plan has been developed, we will use software to show you how your teeth look now and how they will change over the course of treatment. At this appointment we will answer any questions you may have and show you how long treatment will take.
Treatment beings with placement of small, discrete resin ‘handles’ as needed. You will then be given your first set of aligners. The aligners and designed to fit snugly, gently applying force as needed to idealize your bite. Over a few days the ‘tightness’ fades as the teeth move, then the teeth will be ready for a new aligner. The aligners can be easily taken out for meals and for cleaning and flossing.
Does it work? When worn as directed, Invisalign works beautifully! It it is highly effective for cases of mild to moderate crowding and / or rotation [2] Server under – or over – bites may require regular braces. After treatment is complete, retainers must be worn nightly to prevent teeth moving back again.
How long does it take? Cases vary widely; some are minor movements require just 10 weeks but a more typical period is 12 months [3]. Each case is different. The one constant is how happy our patients are with their result. In fact, if you are not happy with your results of a full case, we’ll make the necessary refinement aligners to get things just right.
Share if you care! Please feel free to share this or any Dental Health Matters article and if you have any question, please feel free to email me at doodesdds@gmail.com Who knows, maybe your question will be the subject to another edition!
References:
- John D.Da Silva, Oxford American Handbook of Clinical Dentistry, New York: Oxford University Press, p.162
- Rossini, G et al.,. (Nov 2014). “Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. “.Angle Orthod.
- Fogel, Joshua; Janani, Raymond (2010). “Intentions and behaviors to obtain Invisalign”. Journal of Medical Marketing 10 (2): 135-145.
© Paul Doodes DDS PhD. All rights reserved.
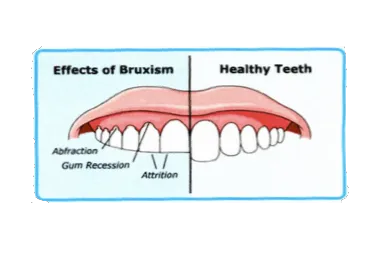
How do I know if I grind my teeth? There are several symptoms that indicate that you may have bruxism (1,3) such as:
- A grinding sound at night, which may disturb the sleep of someone who shares a bedroom with you
- A dull morning headache and or jaw muscles that are tight or painful to open fully
- Damaged teeth, broken dental fillings and injured gums
- Painful jaw joint
- Teeth that are wearing flat
If you have any of these symptoms you may be a bruxer. We will be able to help assess your dentition for signs of bruxism. We will ask about your general dental health, what sources of strss you have in your life, and any medicines you take as some medications induce bruxism (termed secondary bruxism). We will examine the muscles of your jaw, the TMJ function and of course your teeth for evidence of grinding and bite problems. If your bruxism is related to stress, professional counseling may help. You also can try strategies to help you relax. It may help to cut down on stimulants such as tobacco and caffeine.
Can Bruxism be Treated? You do not have to live with the pain, tooth wear or the sound of bruxism. Your partner will appreciate the quiet too! Bruxism can be treated medically (2) or more typically, dentally. We will be able to address the tooth-to-tooth interaction directly by fabricating a custom made occlusal bite splint, also known as an occlusal-guard or night-guard. These devices are ideal for separating the jaw at night (see image). They distribute bite force evenly and allow the teeth to slide easily from side to side preventing the muscle soreness and tooth wear associated with trying to grind tooth cusps over tooth cusps. The appliance takes time to get used to but patients quickley grow comfortable with daily use and welcome the reduction in pain, wear and the improved sleep that they and their partner experience.
Interestingly, 5-5% of children grind their teeth (depending on criteria used for study), mostly in the under 5 age group (4). This typically self resolves as they grow unless it is stress related. Oral appliances of this type are not indicated in children as their jaws are still growing.
An ounce of prevention. Many of you have heard me say “If you cut yourself it will heal, but a hole in a tooth just gets worse”, similarly, continued bruxism associated tooth wear is preventable with early intervention. We can always reconstruct your entire mouth to restore a youthful look and bite, but is far easier to protect the teeth you already have.
Share if you care! Please feel free to share this or any Dental Health Matters article and if you have any questions, please feel free to email me at DoodesDDS@Gmail.com. Who knows, maybe your question will be the subject of another edition!
References:
- J OrofacPain. 2013 Spring;27(2):99-110. Epidemiology of bruxism in adults: a systematic review of the literature.
- Cochrane Database Syst Rev. 2014 Oct 23;10: Pharamacotherapy for sleep bruxism.Macedo CR1, Macedo EC., et al., GFCochrane Database Syst Rev. 2014 Oct 23;10.
- J Orofac Pain. 2013 Winter;27(1):14-20, Temporomandibular disorders, sleep bruxism, and primary headaches are mutually associated. Fernades G et al.
- Dental Press J Orthod. 2014. Nov-Dec;19(6):54-61.,Prevalence of sleep bruxism, in children: a systematic review. Machado E et al.
© Paul Doodes DDS PhD. All rights reserved.
Teeth are made up primarily of two distinct components: The visible white hard outer enamel and the softer yellow dentin that makes up most of the middle and root of the tooth. Both the enamel and dentin are intricate structures that take years for the body to make. Once finished, the tooth, unlike most other parts of the body, can not grow in size or appreciably repair itself. The hard mineralized surface of the tooth makes it ideal for eating with, but also leaves it susceptible to both decay and… chipping.
What usually chips teeth?
Years of daily use. There are not many mechanical things in life as useful and as reliable as teeth; they work with modest maintenance day-in day-out. Yet over the course of many years, after many meals (and often many nights of grinding our teeth in our sleep) fractures appear.
How bad is it?
Fractures or cracks can come in many types or sizes:
Minor cracks – Also called “craze lines,” these are surface cracks. They are very common and typically don’t hurt. However, they can progress into a deeper, more visible and sensitive crack.
Cracked tooth – This type of fracture involves the whole tooth and can become very painful or sensitive.
Chips – Minor chips don’t always need treatment, and can sometimes be smoothed out. As long as it is small and cleansable, it can be left alone ok. Chips on front teeth can be repaired with composite resin and look practically invisible, but due to their location they are susceptible to further chips. Veneers are always an attractive, long-lasting option.
Broken cusp – Cusps can’t be replaced with a filling – they are under too much stress. A stronger restoration is usually needed such as an onlay or crown to encapsulate and support the tooth.
Serious breaks – These breaks go deep enough to expose the nerve. Depending on the case a root-canal-therapy may be needed before a crown is placed. Typically results are very aesthetically pleasing.
Split tooth – This means that the tooth has split vertically and is unrestorable.
Decay-induced break : This is where the tooth has been weakened by decay enough to crumble. By the time decay gets this bad considerable restorative work is required.
Left: Minor chips can be easily restored chair-side. Middle: A serious break, but usually fully restorable. Right: That is not going to buff out – but with crowns and implants, this person will have a great smile again.
What should I do?
Most importantly, don’t panic. This is 2016: We have amazing anesthesia and can reconstruct a tooth beautifully. If you have the fractured part keep it in a plastic bag – it could be useful as a temporary! Call us and we’ll make time for you.
Share if you care! Please feel free to share this or any Dental Health Matters article and if you have any questions, please feel free to email me at doodesdds@gmail.com Who knows, maybe your question will be the subject of another edition!
© Paul Doodes DDS PhD. All rights reserved.
Our teeth are a team that have evolved to work together as a set. Each tooth requires the help of other teeth to stay in place, to function properly and to allow effective cleaning. Take even one out and things start to change. Tooth movement begins after an extraction and is a process that often goes unnoticed until the patient comes in complaining of food trapping and gum irritation under the leaning tooth (See left and center images). Notice also how the opposing teeth have moved down out of alignment with the other teeth. This is especially apparent when a wisdom tooth has continued to erupt without opposition (right image).
What can be done?
Of course prevention is ideal, but if a tooth is lost it can be replaced in a number of ways, ideally before significant tooth movement occurs. It is common to replace missing teeth using:
- Dental implants. Considered the gold-standard in tooth replacement due to their reliable long-term success (1). The artificial tooth root (the implant) is placed and a few months later the implant either restores a single tooth or is used to hold a fixed or removable denture in place securely.
- Bridges can be used to replace a tooth or two by using the neighboring teeth for support. The result is a quick and esthetic replacement; although at least two neighboring teeth have to be altered to allow this method to work. Keep them clean and they are a good long-term solution (2).
- Removable Partial Dentures (RPDs) are a cost-effective way to replace one or several teeth at once. The product clips to neighboring teeth for a good fit but needs to be taken out at night. These products help greatly, but are the least desirable replacement.
If you are living with missing teeth your other teeth are missing necessary support. Restoring missing teeth allows you to fully enjoy your food and to look and feel your best.
Share if you care! Please feel free to share this or any Dental Health Matters article (all available at https://www.myelmhurstdentist.com/dental-health-matters/ ) and if you have any questions, please feel free to email me at doodesdds@gmail.com Who knows, maybe your question will be the subject of another edition!
References:
- Meta-analysis of Failure and Survival Rate of Implant-supported Single Crowns, Fixed Partial Denture, and Implant Tooth-supported Prostheses. Muddugangadhar BC et al.J Int Oral Health. 2015 Sep;7(9):11-7.
- Comparison of Rehabilitating Missing Mandibular First Molars with Implant- or Tooth-Supported Prostheses Using Masticatory Efficiency and Patient Satisfaction Outcomes. Kumar Y., et al. J Prosthodont. 2015 Nov 20
#1 What are E-cigarettes?
E-cigarettes use a small battery powered device to vaporize “Vape” a solution that is then inhaled, similar to a cigarette. The solution can contain either no nicotine, or a specified quantity of the addictive, cancer causing chemical (1).
#2 Are they as dangerous as smoking?
E-cigarettes do not burn tobacco. This alone makes them considerably less toxic than traditional cigarettes (or any tobacco burning product) (1,2). Smoking leaves a residue that stains teeth; vaping does not have a residue so is unlikely to cause stains the same way. It is also much harder to tell if someone has been vaping; there is only a mild odor even when someone is vaping in the same room. This relates to point #3.
#3 Who’s using them?
Disturbingly, the American Journal of Public Health published new data looking at almost 480,000 middle and high school students and found that 24% had tried smokeless tobacco products (3). This is an issue for every parent to be aware of, especially as the long term effects of these products are unknown and many vape fluids contain the addictive cancer causing drug, nicotine. Vaping is a fast growing industry and it’s popularity is not confined to the young. Many people want to ‘smoke’ at work, or in public; some want to quit tobacco smoking (4); some believe it’s harmless and some just like the flavors.
#4 Are they safe?
Safer than tobacco. ENDS are safer than tobacco derived nicotine as other toxic combustion products are not present. However, most vape solutions still contain the addictive, cancer causing nicotine. The effects of the inhalation of the other ingredients in vape solutions are largely unknown (1,2,5). The effects of secondhand vaping is largely unknown.
#5 Are they legal?
Yes, in most places in most states to those over 18. The FDA has begun to regulate the rapidly growing e-cigarette market, however advertising is still unrestricted; this has allowed the development of commercials reminiscent of 1950’s cigarette advertising showing vaping as cool, healthy and safe.
It seems e-cigarettes are here to stay. Eventually, large studies will be performed and we will find the long-term effects of this new delivery system. My concern is that this new twist on cigarettes will create a gateway to nicotine addiction by a generation that is typically repulsed by the sight and smells of burning tobacco in public places. It’s my hope that accurate, science-based, peer-reviewed information will allow us to make sensible personal and regulatory choices.
Share if you care! Please feel free to share this or any Dental Health Matters article and if you have any questions, please feel free to email me at doodesdds@gmail.com Who knows, maybe your question will be the subject of another edition!
References:
- Caponnetto, et al.,”The emerging phenomenon of electronic cigarettes”. Expert Review of Respiratory Medicine 6 (1): 63–74. (2012).
- Cooke, Andrew et al., “The Electronic Cigarette: The Good, the Bad, and the Ugly”. The Journal of Allergy and Clinical Immunology: In Practice3 (4): 498–505.
- G Bostean. E-Cigarette Use Among Never-Smoking California Students. Am J Public Health. 2015 Oct 15:e1-e3.
- Rahman, Muhammad Aziz (30 March 2015). “E-Cigarettes and Smoking Cessation: Evidence from a Systematic Review and Meta-Analysis.” PLoS March 2015
- Rom, Oren et al.,. (2014). “Are E-cigarettes a safe and good alternative to cigarette smoking?”. Annals of the New York Academy of Sciences.
© Paul Doodes DDS PhD. All rights reserved.
Due to continued interest and questions we’ll keep taking a look at some of your questions regarding children’s teeth.
When should I start flossing my children’s teeth?
Toothbrushes, when used carefully and for 2-3 minutes, are great at removing food and bacterial slime (plaque) from teeth. However, they simply do not clean between teeth. The food and slime that remains between teeth irritates gums 24 hours a day eventually causing gum disease and decay between teeth. These two problems have a simple solution: Flossing. Most children have spaces between their baby teeth that allows sufficient cleaning from brushing, however, the molar teeth typically are touching and therefore require flossing. To floss between these 4 sites takes just a few seconds – and you may be surprised to find how much food comes out even after brushing. I floss my daughters teeth once or twice a week – not enough, but enough for her to be familiar with the process.
When to introduce mouthwash / fluoride rinses?
Great question. Flossing is the gold-standard for cleaning between teeth, but mouthwash is a useful way to ensure that loosened bacteria are then prevented from re-settling on the teeth. As soon as your child is able to not swallow toothpaste then it’s a good idea to introduce mouthwash. Rinsing for 30-60 seconds with a fluoride containing mouthwash could become your child’s favourite part of the morning/nighttime routine!
Does my child need sealants?
Perhaps. Sealants are an effective, non-invasive, long-lasting way to minimize the risk of the most common type of tooth decay (cochrane 2004) . However, we don’t recommend them to everyone. If the child has great oral hygiene, no previous decay and easy to clean tooth anatomy (no deep grooves or pits) then the’ll be fine without them.
How safe are dental x-rays for my child?
Technological advances in x-ray devices have allowed modern dental offices like ours to reduce exposure to radiation significantly.
Are thumbsucking and pacifier habits harmful for a child’s teeth?
Eventually, yes. Thumbsuckers and pacificer users and ‘tounge-thrusters’ can, over time, develop excessively protruding front teeth that can’t bite (see image for an extreme example). Minor open bites are normal as the teeth transition from child to adult teeth and most self-correct, however, early assessment and preventive measures are important to reduce likelihood of protracted use of braces.
Many thumb-sucking gadgets and even dental appliances are available to break the habit. If in doubt, ask your dentist.
When should I take my child to see an orthodontist?
Straight teeth don’t just look better, they work better as a group and are easier to clean leading to better dental and gum health. The American Association of Orthodontists (3) recommends an initial visit to an orthodontist by the age of 7. Why so early? Some problems are best addressed early to minimize the extent of intervention later. Most children do not require early intervention, but an orthodontist is able to provide you a path to straight teeth and the initial consultation is typically at no charge, so you’ve got nothing to lose.
Why are school forms necessary?
Students miss more than 51 million school hours per year (4) because of dental problems or related conditions. Tooth decay and gum disease are largely preventable and are easy to transmit to other people as they are bacterially mediated. We all share spoons, drinks, and food and therefore we allow the transmission of oral bacteria from person to person, especially within a family or caregiver to child. This is why we talk of good habits for the whole family.
It’s my hope that with accurate, science-based, peer-reviewed information we can help ensure that our children grow up without the most common childhood infection – cavities (4).
Please feel free to share this or any Dental Health Matters article and if you have any questions, please feel free to email me at doodesdds@gmail.com Who knows, maybe your question will be the subject of another edition!
References:
- Law V., et al. Aust Dent J. 2007 Jun;52(2):93-100; quiz 159
- Ahovuo-Saloranta et al., Cochrane Database Syst Rev. 2004;(3):CD001830
- American Association of Orthodontics (www.aaoinfo.org)
- US DHHS: Oral Health in America: A Report of the Surgeon General. Rockville, MD: NIDCR, NIH; 2000
© Paul Doodes DDS PhD. All rights reserved.
Last month we started to take a look at dental care for young children. This month we continue this important topic by addressing more common questions:
- How long should I brush for? We’re all familiar with the 2 minutes 2 times a day mantra, but how does this relate to children’s teeth? Children have shorter attention spans than adults, to them 2 minutes may as well be 2 hours. While opinions vary (1), it’s worth knowing most adults brush for just 45 seconds and that there are significant improvements to be had from longer brushing sessions and from electronic toothbrushes (2,3).Realistically, I suggest determining how long your child will tolerate you cleaning his/her teeth and divide that number by 4 and spend that much time on each quadrant, focusing on the biting surfaces at first the most common surfaces to get decay. Again, stick to the Mommy/Daddy brushes first concept to address difficult areas while you can!
- When should I take my baby in to see the dentist? The American Academy of Pediatric Dentistry recommends that you take your child to the dentist within six months after her first tooth erupts, or by her first birthday, whichever comes first (3). The early visits are helpful mostly because of parent / caregiver education. However, each dental practice has it’s own preference; many, like ours, suggest by 3 years old unless there is an obvious problem.
- It’s not just sugar that’s bad! We are all familiar with hearing the evils of sugar, but what is more surprising is how many foods contain either sugar or other fermentable carbohydrates that also fuel the bacteria that make decay causing acids. Frankly, most foods and drinks contain either sugar or related simple carbohydrates. Foods such as bread, crackers, chips, pasta and rice all quickly breakdown when sitting on and in between the teeth. Essentially all foods contribute to the acidic environment that causes tooth decay. Notable exceptions are water and most cheeses (note that Kraft Singles are not legally allowed to be labeled as cheese but merely a “Pasteurized Processed Cheese Product”). Even milk contains plenty of sugar, so make water the drink for between meals. Instead of obsessing about limiting candy and soda,consider trying to decrease frequency of snacking: Eat a meal. Don’t eat for a few hours. Repeat.
Aren’t they just baby teeth? Some parents think baby teeth aren’t important because they’re eventually replaced by permanent ones; but these first teeth preserve the spacing for the permanent ones and help your baby chew and talk. They also allow children to develop good oral hygiene habits.
The slow transition from children’s teeth to adult teeth allows the same bacteria to stick around into adulthood. This is why children with cavities tend to become adults with cavities (4, 5).
As your baby grows older you can introduce regular tooth brush cleaning at around 12 months with a rice grain sized portion of regular toothpaste (5). Fluoride containing toothpaste has a long track record of reducing decay rates, and is supported by many welldocumented studies (6).
- It’s my hope that with accurate, sciencebased, peerreviewed information we can help ensure that our children grow up without the most common childhood infection cavities (5).Please feel free to share this or any Dental Health Matters article and if you have any questions, please feel free to email me at doodesdds@gmail.com Who knows, maybe your question will be the subject of another edition!
References:
- Inconsistencies in Recommendations on Oral Hygiene Practices for Children by Professional Dental and Paediatric Organisations in Ten Countries. Int J Paediatr Dent. 2011 May;21(3):2233
- The Effect of Brushing Time and Dentifrice on Dental Plaque Removal in vivo. J Dent Hyg. 2009 Summer;83(3):1116. Epub 2009 Aug 14
- Powered Versus Manual Toothbrushing for Oral Health. Cochrane Database Syst Rev. 2014 Jun 17;6:CD002281. doi: 10.1002/14651858.CD002281.pub3
- US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000
- American Academy of Pediatric Dentists ( www.AAPD.org )
- Fluoride Toothpastes for Preventing Dental Caries in Children and Adolescents. Valeria CC Marinho et al. Cochrane Library Jan 2003.
© Paul Doodes DDS PhD. All rights reserved.
It’s natural for a parent to worry about how to best look after their children’s teeth. As a dentist and a father of two young children, I’ve been mentally compiling a list of questions from many worried parents and answers from reputable sources. We get so many questions related to children’s teeth that I’ll be continuing this article in the future.
Here is a list of 5 ways you can help ensure a healthy start for your children’s teeth:
- Family culture: My first piece of advice is it make good oral hygiene habits part of your family culture; when children see that their parents brush twice a day – or maybe three times if they are at home for lunch – the children take this on as just something that ‘we do’. Like many things, this is simple but not easy as we are all in a rush in the morning, but it can be done and in my opinion makes a profound difference. In the same way that “We don’t hit each other”, “We say please and thank you” become part of your family culture so can “We brush (and floss) twice a day”.
- Make it fun! Having your young children see you brush your teeth helps. Having your young children see you brush with a smile really helps. I’ve heard parents really sing the praises of this simple change. When children see you happily brushing your children will want to take your brush and start themselves. Sing a song while brushing! Do a dance! Whatever you like just ensure your children see you brushing and enjoying it.
- Minimal Toothpaste: Ignore the big stripe of toothpaste on the commercials; we really don’t need much toothpaste. It’s great tasting, improves the feel of the brushing process, improves our breath and in almost all cases contains a small amount of fluoride to help strengthen areas of teeth that our diets and habits have allowed to become weaker. I just dip the tips of the bristles in the paste and it foams up nicely. Less to swallow, less to worry about. The American Academy of Pediatric Dentists (1) recommends a ‘rice’ sized amount up to 3 yrs and a pea sized amount thereafter.
- Daddy/mummy brushes first:/strong> Children – and adults – have limited attention spans. Seize the moment and get the most decay-prone areas clean first because your child will soon want to be finished. What areas? Back teeth. Commit to cleaning the biting surfaces of all back teeth, top, bottom, left and right for about a quarter of the time that your child could last tolerate you brushing. By cleaning the back teeth first, then having the child ‘bite’ and brushing the outside all around you’ll have done the lion’s share of the cleaning. Then hand over the brush to Timmy to have fun.
- Rinse / Spit: Children are notorious for swallowing toothpaste and mouthwash. However, even my 20 month old can rinse and spit fairly well. How? I demonstrate rinsing and spitting. He finds it hilarious to watch me spit into the sink so he tries to copy me. He’s not ready to spit across the room yet, but he’s getting there. If you’re using a small amount of toothpaste there’s less to worry about with regards to swallowing. The American Academy of Pediatric Dentists now recommends using a tiny amount of regular toothpaste for children of all ages (1,2)
- Next month we’ll continue to explore the topic of children’s teeth. It’s my hope that with more accurate, science-based, peer-reviewed information we can help ensure that our children grow up without the most common childhood infection – cavities (3).
Please feel free to share this or any Dental Health Matters article and if you have any questions, please feel free to email the office at info@cottagehilldentalcare.com . Who knows, maybe your question will be the subject of another edition!
References:
- AAP Recommends Fluoride to Prevent Dental Caries – August 24th 2014.
- Fluoride Use in Caries Prevention in the Primary Care Setting, Melinda B. Clark, MD et al. American Academy of Pediatrics. Pg 626
- US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000
© Paul Doodes. All rights reserved.
Firstly, let’s define whitening. Whitening is any process that makes teeth appear whiter. Simple. However, there are two approaches: One is non-bleaching whitening, which is to say, removing surface stains. This is akin to scrubbing a dirty floor to see the original color come through. The second way is using bleaching products(1). These bleaching products change the actual color of the enamel and can remove surface stains too. As such tooth whitening has the ability to turn back the clock on your teeth – quickly and easily removing decades of staining from foods and drinks.
Tooth whitening goes back to ancient times with the Egyptians known to use various concoctions – including urine – of dubious merit. As little as 200 years ago services were available to file stained enamel from teeth and to treat with nitric acid to whiten, this worked, but also led to pain and decay(2). I won’t waste another word on ancient techniques; if they were effective, we’d still be using them.
In the 21st century, there are many over-the-counter products available and all work on a similar principle: The active ingredient, an oxide such as carbamide peroxide, is suspended in a gel that is applied to the teeth. The active ingredient oxidizes stains and reveals the natural shades and translucency(1). Some of the over-the-counter products can work well, but nothing matches custom trays made by a dental professional for the fit and contours that whiten all the way to the gum line.
By contrast whitening toothpastes are typically abrasive forms of regular toothpastes. These can be helpful in removing surface stains in people who smoke or drink a lot of tea/red wine. However, they only remove surface stains, not intrinsic stains as the bleaching products do. Many people want a brighter, more youthful smile but are concerned that they’ll end up looking like George Hamilton. Relax, the milder whitening gels take many hours to work and you can stop at any time or decide to keep going; it’s up to you!
Whitening works very well for most people and can in some cases reduce the visibility of ‘fluorosed’ teeth by minimizing the contrast between the different colors of the teeth. It is best to consult a dentist before embarking on this treatment due to the potential for exaggerating the appearance of stains, leading to frustrating results and expensive corrective treatment. This is why it’s important to have a dentist assess your dental health before beginning whitening treatments.
The most common problem with whitening is tooth sensitivity during or after treatment. If your teeth are sensitive to hot or cold you may benefit from using a desensitizing toothpaste for a few weeks before and after bleaching to minimize any sensitivity. Non-steroidal ant-inflammatory drugs such as Advil or Aspirin also help eliminate any ‘zing’ of sensitivity. The second most common problem with over-the counter products is that people don’t realize that their restorations (crowns and fillings) do not whiten at all. This creates a discrepancy in tooth color and can be both frustrating an expensive to fix. Bleaching products are highly effective and have been the subject of many, many scientific studies to establish their efficacy, safety and long term effects on teeth. Does whitening cause dental decay? No(4)
To conclude, is there any truth to any of the accusations against tooth whitening? Published scientific papers show modest demineralization immediately after whitening, but tooth strength was normalized moments later thanks to salivary minerals (3). Tooth sensitivity can be bothersome to some, but typically self-resolves. The effects of whitening can last for years depending on how your teeth respond to stains, how they respond to the whitening and what you eat. Those who love tea, red wine and coffee seem to pick up the most stains, with tea the worst offender (and I ought to know). We get used to our bodies aging each year; tooth whitening gives us the opportunity to remove decades of stains to reveal a youthful smile.
So, why not give it a try? I’m confident you’ll love the results!
Paul Doodes DDS, PhD.
References:
1) NJ Dent J 2013 Sep; 109(3): 87-96. Elfallah HM et al.
2) Northwest Dent. 2010 Nov-Dec; 89(6): 19-21, 23-6. Perdigao J
3) J. Evid. Based Practice, 2014 Jun; 14 Suppl: 70-6. Carey CM
4) Oper Dent 2005 Mar-Apr; 30(2): 265-70. Al-Qunaian TA
What puts someone at risk for oral cancer?
Risk factors include:
- Age (typically over the age of 40)
- Tobacco use (cigarettes, cigars or chewing tobacco)
- Excessive alcohol consumption
- Persistent viral infections, such as HPV16
- A poor diet (lacking or low in fruits and vegetables)
Wouldn’t I notice oral cancer?
Not necessarily. Oral cancer can go unnoticed early as there are very few signs or pain mark the early stages of oral cancer. However, some early abnormalities are easy for a professional to spot:
- White or red patches of tissue
- Small ulcers that resemble canker sores that don’t go away
- Lumps or masses in the mouth or neck
- Wartlike masses
- Sores or discolorations that don’t abate within 14 days
- Pain when swallowing, chewing, or speaking
- Numbness of the mouth or face
Early detection is simple, painless and important. When treated early, survival rates are much higher. If cancer has metastasized to multiple areas, intervention will be more involved.
How can I prevent oral cancer?
Aside from receiving an oral cancer screening during your dental exams, there are many things you can do to help prevent oral cancer including: only drinking alcohol in moderation; enjoying a healthy diet; limiting your exposure to the sun and always wearing UVA/Bblocking lotions on your skin and lips.
What is the survival rate?
Sadly, survival rates of oral cancer are not good; only about 57% of patients survive past 5 years. This is why prevention is so important. Thankfully, early detection is relatively easy as the mouth is so accessible. Even if you don’t have any risk factors you are still at risk, so be sure to visit your dentist regularly and ask for a cancer screening.
Paul Doodes DDS, PhD
References:
//oralcancerfoundation.org
We get a lot of questions about Botox Cosmetic™ treatments at the office, so I thought it may be helpful to answer some questions and to perhaps dispel some common misconceptions that people may have.
Botox Cosmetic has been used since the 1980’s to successfully treat muscle disorders of the eye (1). Soon after, plastic surgeons began using it to treat cosmetic wrinkles (2).
The rest is history. Millions of injections later, Botox is revered as a medical success story. Dr. Matthew Avram, director of the Dermatology Laser and Cosmetic Center at Massachusetts General Hospital recently opined that “Botox truly stands out as a safe and effective treatment that has revolutionized the way we can achieve facial rejuvenation”(3).
Here are some answers to some common questions:
What is Botox? Botox cosmetic is a highly purified natural protein that relaxes the muscles that causes wrinkles. Injections are using a tiny needle and results are seen in a few days. This means those pesky wrinkles will be minimized or eliminated . . . for 3-4 months!
Isn’t Botox a toxin? Yes. Botox is a highly purified naturally occurring toxin produced by the bacteria Clostridium botulinum, most commonly found in the soil, including in the Midwest. Tiny doses placed carefully by well-trained practitioners make amazing results possible.
How long does it last? Typically 3-4 months. Interestingly, after 3-4 months a second application of Botox will reveal even better results! This is because the skin has been relaxed already and then continues to relax.
What areas do you treat? The most common areas of concern are the “11’s” between the eyes, horizontal forehead wrinkle and “Crows feet”.
Are there any people for whom Botox isn’t a good idea? Yes, but not many people are poor candidate. We don’t treat people who are pregnant or lactating, people with muscle disorders, skin infections or those who have allergies to components of the solution.
Are Dysport and Xeomin as good as Botox? Great question. They are similar products derived from the same bacteria. They work comparably well. We just prefer to work with a product that has worked so well for us, and is backed by almost 20 years of success.
Why is dentist placing Botox? Because we have a detailed knowledge of facial anatomy, muscles and injection techniques! Plus, the visit is quick, almost painless, and discreet – you can go back to work after your treatment. With a unique combination of knowledge of medicinal chemistry (BSc), dentistry (DDS), immunology/microbiology (PhD) and hands-on training from #1 provider of Botox in North America, I feel ideally trained and experienced to administer Botox.
How many units do I need? Good question. The only way we can determine this is by taking a close look at you and asking “How can we help?”. Most people are concerned with lines on the forehead, around the eyes and between the eyes – great areas to treat with Botox for a relaxed, refreshed look. The number of units is determined by your anatomy and your wants. Typically we treat with modest doses at first, and then if you like, we add more to ensure you’re thrilled with the result.
Will Botox work for me? Most likely, yes! The best way to find out is to call and book a consultation where we can discuss your concerns and see if Botox is right for you! I hope this answers some of your questions. If you still have questions, please come in for a consultation; I’d be happy to talk to you.
Paul Doodes D.D.S., Ph.D.
References:
- Flanders et al. CJO (22)4 pages 212-217
- Clarke RB et al., PRS 84(2) pages 353-355
- “Americans Stuck on Botox”, USA Today, 4/11/2012
New Research Reveals Smoking is good for your health!
We are all used to the negative press smoking gets, so it was a surprise this week to see that data now supports smoking as an adjunct to brushing and flossing.
APRIL FOOL!! Of course smoking is bad for your teeth; in fact, it causes a mouthful of trouble. A full 1 in 5 deaths are tobacco related. That’s a huge number of preventable deaths each year, about 480,000 in the USA alone.
A common misconception about smoking is that it mostly kills from causing cancer; in reality, it kills more people from heart disease. This is due to nicotine. Nicotine is the addictive drug in tobacco products that causes the heart to race and small blood vessels to constrict. When this happens, it stresses your heart and when used regularly, can lead to heart disease which is the leading cause of death in the USA for both men and woman.
The Centers for Disease Control and Prevention (CDC.gov) states that a full 9/10 people that die from lung cancer have smoked and that 8/10 people have died from chronic obstructive pulmonary disease have smoked.
Let’s remember how addictive nicotine products are. If the awful statistics, foul breath, yellow teeth and gum disease aren’t enough to persuade you to quit, please talk to your physician or dentist about prescription medications that can minimize the desire to smoke.
Your health is important to us. Please consider the source of your healthcare information! CDC offers a wealth of science-based peer-reviewed information on may health topics (CDC.gov).